 Documents for Discussion
Documents for Discussion
You can use the Documents for Discussion section to review clinical documents related to a patient, including results, open patient cases with clinical questions, orders that were submitted but have not been associated with a result, and open inbound clinical documents. You can also use the Documents for Discussion section to record that you discussed a document with a patient during an encounter.
This section does not include documents created in the current encounter, such as point-of-care tests; athenahealth recommends that you review these documents elsewhere in the encounter workflow, such as the Assessment / Plan section.
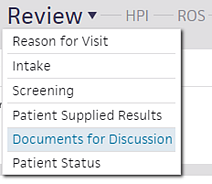
In the Exam stage of the encounter, click the Review down arrow and select Documents for Discussion.
- In the Exam stage of the encounter, click the Review down arrow and select Documents for Discussion.
- Click the document to display it.
- To close the document, click the X at the upper right.
- After you discuss a document with the patient, mark the document as discussed by clicking the checkbox to the left of the document.
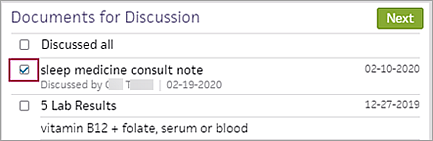
Note: If you clear the checkmark for a document that is marked as "discussed" and the document was set to CLOSED status, the document is reopened in REVIEW status. -
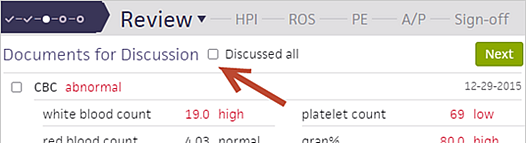
You can also use the Discussed all checkbox at the top of the list to mark all documents as discussed.
Note: If all the discussed documents were assigned to you, they are automatically closed. For information about whether documents not assigned to you are closed, see Closing documents that are marked as discussed with the patient.
You can mark an encounter as a transition of care encounter in the Reason for Visit step of the Intake checklist or in the Review step of the Exam stage. The best practice is for an MA, nurse, or other staff to mark the encounter as a transition of care encounter during the Intake stage.
Note: For more information, see Transition of care documents and the Medicaid PI HIE measure on the Summary of Care Record/Continuity of Care Document page.
Before you begin the Exam stage, review the Quality tab, which displays HIE Receive and Incorporate measure details for encounters marked as transition of care. "Needs data" indicates that you must discuss the electronic summaries related to transition of care with the patient during the exam. athenaOne removes the measure from the tab after you satisfy the measure.
- To begin the Exam stage, click Go to Exam in the upper right corner of the screen.
The Newly referred patient or a patient being referred back option appears in the Reason for Visit section. - Confirm with the patient that this encounter is a transition of care. If the Newly referred patient or a patient being referred back option is not selected, select it now.
Note: If the encounter is not a transition of care, deselect the Newly referred patient or a patient being referred back option if this option is selected. - Scroll down to Documents for Discussion.
Electronic summaries related to the transition of care are listed.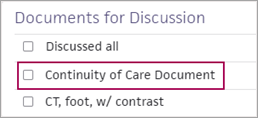
Note: Documents labeled "Summary of care," "Continuity of care," "Referral note," or "Discharge summary" satisfy the HIE: Receive and Incorporate measure. Any other documents related to a transition of care that appear in the Documents for Discussion section do not satisfy the measure.
If transition of care documents are available
- Discuss each summary of care document with the patient.
- Check the box next to each document after you review it, or check the Discussed all box.
If transition of care documents are not available
- If no transition of care documents are available for this encounter, specify whether you requested the document from the provider.
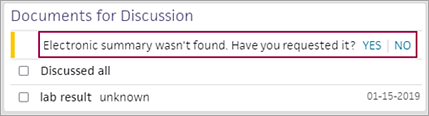
- Electronic summary wasn't found. Have you requested it? — Select an option.
- Click Yes if you contacted the organization that the patient is coming from to request the summaries in CCDA format. The encounter is excluded from the HIE measure.
Note: Keep the encounter open until you receive the transition of care documents. Return to the encounter and select YES when you receive the documents. - Click No if you will not contact the organization that the patient is coming from to request a transition of care summary. The HIE measure is counted as unmet for this encounter.
After you complete the Exam stage, "Transition of Care Encounter" appears in the encounter summary and the full encounter summary.
For a single-specialty practice, this section displays documents from the day after the patient's last visit through the current date.
If your practice uses the Multispecialty Filtering feature, this section displays documents from the day after the patient's last visit with the rendering provider's specialty, if available, through the current date. If the rendering provider's specialty isn't available, or the patient has no visits with the specialty of the rendering provider, this section displays documents from the day after the patient's last visit at the practice through the current date.
Note: All result documents that aren't closed appear, regardless of the date range, to ensure that you have full visibility of a patient's results.
Before the Summer 2020 release, athenaOne automatically closed a discussed document in the Clinical Inbox after any user marked the document as "discussed" in the Documents for Discussion section of the Exam stage. Your practice can request that discussed documents be automatically closed only when:
- The document is open and assigned to the rendering provider.
- The rendering provider discussed the document with the patient and marked the document as "discussed" in the Documents for Discussion section.
Documents that are not assigned to the rendering provider remain open in the Clinical Inbox so that the person assigned to that document can take the appropriate action on it, even if the rendering provider marks the documents as "discussed" in the Documents for Discussion section.
To request this behavior in the Documents for Discussion section, please submit a case to the CSC from athenaOne > Support > Success Community > Contact Client Support Center.
Note: If your practice began using the athenaClinicals service after July 2020, this behavior was enabled for you, and you do not need to take any action.
Transition of care is the movement of a patient from one setting of care to another (settings of care include hospital, primary care practice, specialty care practice, long-term care, home health, and rehabilitation facility).
The Promoting Interoperability programs includes the Health Information Exchange (HIE): Receive and Incorporate measure. This measure calculates the percentage of transition of care encounters that are linked to an electronic summary in Consolidated Clinical Document Architecture (CCDA) document format.
Note: Information for the HIE: Receive and Incorporate measure appears on the Pay for Performance Dashboard under the PI Medicaid - 2019 (Behavioral 90 day) program bar.
To satisfy the HIE measure for transition of care documents, a summary of care record or continuity of care document must meet these specifications:
- The document is in Consolidated Clinical Document Architecture (CCDA) format (see Summary of Care Record/Continuity of Care Document).
- The document has not been deleted.
Note: Closed electronic summaries appear in the Documents for Discussion section only at the patient's first visit after the document arrived. - The document has not been selected in another encounter.
The following electronic summaries linked to transition of care encounters satisfy the HIE: Receive and Incorporate measure:
- Summary of care records
- Continuity of care records
- Referral notes
- Discharge summaries
Note: Other documents related to transition of care may appear in the Documents for Discussion section of the Exam stage. athenahealth recommends that you review these documents as you provide care, but these documents do not satisfy the HIE: Receive and Incorporate measure.
Transitional care management (TCM) encounters are follow‑up visits after a patient is discharged from one of these facilities:
- Hospital
- Long-term care center
- Rehabilitation
- Skilled nursing
Every TCM encounter is a transition of care encounter, but transition of care encounters also include newly referred patients and patients returning to a provider after completing care that the provider referred them to.
You can find transition of care documents using the Find tab in the patient chart and in the Clinical Inbox. You can also use the Document Search page:
- Document Class — Select Clinical Document.
- Document Subclass — Select Record of Care.
Before you begin the Exam stage, athenahealth recommends that you review the Quality tab. The tab displays HIE Receive and Incorporate measure details for encounters marked as transition of care.
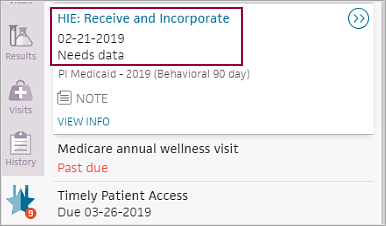
"Needs data" indicates that you must discuss the electronic summaries related to transition of care with the patient during the exam. athenaOne removes the measure from the Quality tab after you satisfy the measure.
The transition of care workflow satisfies the Health Information Exchange (HIE): Receive and Incorporate measure of the Medicaid Promoting Interoperability program. To satisfy the measure, your organization must complete these tasks:
- During the Intake or Exam stage of the encounter, mark the encounter as a transition of care (see To mark an encounter as a transition of care encounter).
- During the Exam stage of the encounter, review and discuss the electronic summaries related to the transition of care with the patient (see To complete transition of care documentation during the encounter).
Note: A return encounter counts toward the current year's quality measure reporting, even if a patient returns to your organization after completing care that you referred them to in a prior year.
You are required to complete the transition of care workflow if your organization participates in Medicaid Promoting Interoperability programs. If your organization does not participate in Medicaid Promoting Interoperability programs, you can turn this feature off by opening a support case or by contacting your Customer Success Manager.
Important: If you turn off this feature and then later decide to report on the HIE measure, you cannot capture transition of care data retroactively.